Welcome to the March 2024 North Dakota Medicaid provider newsletter and thank you for caring for our members.
“Never believe that a few caring people can’t change the world. For, indeed, that’s all who ever have.” - Margaret Mead
Ordering/Referring/Prescribing Provider Claim Requirements
Effective for dates of service May 1, 2024, and after, ND Medicaid will require that the ordering/referring/prescribing (ORP) provider’s individual National Provider Identifier (NPI) be present on all 837P transactions (professional claims) for the following services.
- Behavioral Health Rehabilitative Services including:
- Behavioral Intervention
- Individual and Group Counseling
- Intensive In-Home for Children
- Nursing Assessment and Evaluation
- Skills Integration
- Skills Restoration
- Diagnostic Services including:
- Audiologic Function Tests
- Diagnostic and Screening Laboratory Services
- Diagnostic and Screening Radiology and Imaging Services
- Echocardiograms
- Electrocardiograms
- Electronic Analysis or Interrogation of Implanted Devices
- Neurodiagnostic Services (EEG, VEP, EMG, Polysomnography)
- Pulmonary Function Studies/Testing
- Psychological and Neuro-psychological Testing
- Eyeglasses frames, lenses and contacts
- Durable Medical Equipment and Supplies
- Hearing Aids
- Occupational Therapy Services
- Physical Therapy Services
- Physician Administered Drugs (any drug administered in the clinic setting)
- Preventive Services including:
- Immunizations
- Preventive Evaluation and Management Services
- Well-Child visits
- Adult Preventive Exams
- Counseling for Risk Factor Reduction
- Tobacco Cessation
- Prosthetics
- Speech Therapy Services
Read the Ordering/Referring/Prescribing Providers policy to learn about which provider types may be ORPs and other requirements. The policy also contains a FAQ section.
ND Provider Contacts

Provider Enrollment
Call (701) 277-6999 between the hours of 9 a.m. – 3 p.m. CT Monday through Friday to speak to an enrollment specialist. Leave a message after these hours. You can also email NDMedicaidenrollment@noridian.com with questions or for support.
Note:
- Developmental Disability Providers call (701) 328-8935 or (800) 755-8529.
- Qualified Service Providers call (701) 328-4602 or (800) 755-2604.
Provider Relations Call Center
Call (701) 328-7098, toll-free (877) 328-7098 or email mmisinfo@nd.gov when you have questions about member eligibility, payments, denials or general claims questions.
Pharmacy
Call (701) 328-4086 with pharmacy claims questions and (701) 328-4023 with program questions or email medicaidpharmacy@nd.gov.
Health Tracks
Call the Health Tracks Provider Outreach Team at (701) 328-2014 (then press 2) or email HTprovideroutreach@nd.gov with questions about our Health Tracks/EPSDT benefit.
Durable Medical Equipment (DME)
Call (701) 328-2764 or email tamholm@nd.gov with questions about DME or supplies. For billing questions, call the Provider Relations Call Center.
Third Party Liability
Call (701) 328-234, toll-free (800) 755-2604 or email medicaidtpl@nd.gov for questions about third party liability, private insurance or Medicare.
Medicaid Expansion – Blue Cross Blue Shield of North Dakota
Call (833) 777-5779 with questions on Medicaid Expansion.
Medicaid Fraud/Abuse
Report suspected fraud by providers or members by calling (800) 755-2604, emailing medicaidfraud@nd.gov or completing the Surveillance and Utilization Review Section (SURS) Referral Form.
Service Authorization Contacts
See who to contact for services requiring service authorizations here.
Coordinated Services Program
Call (701) 328-2346, toll-free (800) 755-2604 or email medicaidcsp@nd.gov with questions about the Coordinated Services Program.
Other Questions
Call the Medical Services Division at (701) 328-7068, toll-free (800) 755-2604 or email dhsmed@nd.gov with other questions you may have.

Did You Know? ND Medicaid member eligibility reviews
ND Medicaid members must have their Medicaid eligibility reviewed every 12 months.
Medicaid has automated reviews where we have access to a member’s information through available databases.
If we are unable to automate the review, a pre-populated review form is sent to members. To determine ongoing eligibility, the member must review and update any changes on the review form and return it to the address on the form along with proof of the changes.

Sports physicals are covered and easy to incorporate into well-child visits
Our Health Tracks team wants to thank our clinical providers for their work on including well-child visits with sports physicals.
Since the sports physical code went live July 2022, ND Medicaid has seen:
- 883 sports physical claims
- 2,312 well-child visit claims that included a sports physical
- 1,387 office (non-well-child visit claims) that included a sports physical
The sports physical code that is covered by ND Medicaid is CPT© code 99429 along with ICD-10 code Z02.5.
It’s easy to convert a sports physical to a well-child visit!
Since many teenagers go several years between checkups, it is important to increase our number of Medicaid-eligible teenagers getting preventive well-care services.
How can providers help keep the momentum going?
Simple! When a family calls your office for a sports physical appointment, encourage them to schedule a well-child visit at the same time. This ensures they are healthy both on and off the field.
To find information, including the sports physical form, visit the North Dakota High School Activities Association forms webpage.
Learn more about Health Tracks.
Lead Screening 
Did you know blood lead screening is required for all children enrolled in ND Medicaid at ages 12 months and 24 months?
ND Medicaid-enrolled children between ages 36 and 72 months should have a blood lead test if they have not been previously screened for lead exposure.
Children living in homes built before 1978 are at an increased risk of lead-based paint exposure and should be screened. In North Dakota, over 50% of households were built before 1978.
Lead screening code is covered by ND Medicaid under CPT® code 83655. This is a preventive code and does not require a primary care provider referral.
How can providers help?
Screening our youngest ND Medicaid members for lead helps prevent lifelong negative impacts. Lead screening results can be reported to the North Dakota Office of the State Epidemiologist by mail at 600 E. Boulevard Ave., Bismarck, ND or by fax (701) 328-2785.
For more information, visit hhs.nd.gov/health/lead or contact the state Lead Program at mnovosel@nd.gov.
 Dental screening and assessment limit changes
Dental screening and assessment limit changes
Effective March 1, 2024, ND Medicaid is expanding its coverage of dental assessments and screenings to include two services per year. This could be two dental assessments OR two dental screenings per year OR one of each service per year.
Members are limited to receiving a combined total of two services using the below codes.
- D0190 – screening of a patient
- D0191 – assessment of a patient
Attn: Organization administrators - deactivating inactive user accounts

It is the responsibility of the organization administrator to self-manage their staff members’ user account access to the MMIS Web Portal.
The department strongly encourages all ND Medicaid providers to establish, at a minimum, one primary and one back-up organization administrator.
Effective Feb. 10, 2024, if a user’s account has not been active in 365 days, the MMIS Web Portal system will automatically terminate the user’s account.
Questions? Call the Provider Relations Call Center at (701) 328-7098, toll-free (877) 328-7098 or email mmisinfo@nd.gov.
 Changes approved for home and community-based behavioral health supports and services through the Medicaid 1915(i) State Plan Amendment and for the Autism Waiver
Changes approved for home and community-based behavioral health supports and services through the Medicaid 1915(i) State Plan Amendment and for the Autism Waiver
Qualifying ND Medicaid members with autism and certain behavioral health conditions have increased service accessibility and more services thanks to two recent approvals from the Centers for Medicare and Medicaid (CMS).
The Medicaid 1915(i) State Plan Amendment allows ND Medicaid to pay for in-home and community-based services for eligible individuals. The program serves individuals of all ages with mental illness, substance abuse disorders, and/or brain injury and is designed to keep individuals out of institutional settings with in-home and community-based services for successful independent living.
Effective Feb. 1, 2024, a Medicaid 1915(i) State Plan Amendment was approved by CMS to add an additional needs-based assessment for member eligibility: the Daily Living Assessment-20 (DLA). Eligible members require a score of 5 or lower. It’s estimated 730 individuals will qualify for Medicaid 1915(i) services with a DLA score of 5 or lower. Only DLAs administered through any of ND’s eight regional human service centers are accepted for Medicaid 1915(i) eligibility.
Other approved revisions include changes to provider qualifications for care coordination, benefits planning, prevocational training, supported employment and supported education; revisions to eligibility requirements in an effort to serve more ND Medicaid members; increased remote support service limits; removal of annual service limits; allowance of retroactive service authorizations and modifications to the conflict of interest exceptions. Learn more about Medicaid 1915(i).
The state's Autism Spectrum Disorder (ASD) Waiver was renewed effective Nov. 1, 2023, and now serves youth birth through age 17. It includes increased waiver slots to serve more members. Two new services were added – remote monitoring and community connector. Remote monitoring is a GPS device to assist in locating a child that has severe wandering behaviors and community connector will allow for a child with ASD to attend and participate in their community with the goal of building relationships and natural supports.
Additionally, the waiver renewal allows for the enhancement of service management to include a rural differential rate for providers assisting rural families access waiver services. This rate is for time spent at the home of the waiver participant and is based on total miles from agency to the home.
Any agency interested in providing service management through the ASD waiver can reach out to Katherine Barchenger, Children’s Waiver Administrator at (701) 328-4630 or by email kbarchenger@nd.gov for more information.
Seeking Medicaid Member Engagement Committee (MMEC) and Medicaid Member Advisory Committee (MMAC) members 
We are looking for members to serve on two important ND Medicaid committees.
Medicaid Member Engagement Committee (MMEC)
| Medicaid Medical Advisory Committee (MMAC) |
This committee is made up of current and former Medicaid members and their caregivers (recipients within the last three years). | This committee is made up of current and former ND Medicaid members (recipients), providers who serve ND Medicaid members, legislators and others with relevant experience. |
Members are invited to share their Medicaid experiences and ideas for improvement. | Members advise ND Medicaid on health and medical care services. |
Interested members can contact Member Liaison Jen Sheppard at medicaidmembers@nd.gov or learn more about the MMEC including how to apply at hhs.nd.gov/medicaid-member-engagement/committee.
The MMEC is currently accepting applications on an ongoing basis. | Interested individuals can apply by May 7.
Email the following information to the ND Medicaid Director:
Learn more about the MMAC or email Mandy Dendy at mrdendy@nd.gov with questions. |
Chiropractic Providers 
The Chiropractic Services policy has been updated to provide clarification.
- Only chiropractic manipulative treatments (CMT) of the spine are covered (CPT 98940-98942). Extraspinal chiropractic manipulation (CPT 98943) is not covered.
- Covered x-rays are limited to cervical, thoracic, thoracolumbar or lumbosacral portions of the spine. X-rays are limited to two per region per calendar year. X-rays of the hip, pelvis or extremity are not covered.
- Chiropractic claims require the submission of two ICD-10-CMT codes to support medical necessity. The primary diagnosis must be the level of subluxation AND the secondary diagnosis must be the associated neuromusculoskeletal condition.
- Chiropractic spinal manipulation codes are limited to 20 per calendar year. Any additional manipulations require a service authorization.
- Services listed as not medically necessary in the guidance will not be covered.
Incontinence Supplies Policy 
ND Medicaid’s Program Integrity Unit is required to conduct post-payment claims audits.
One of the audits conducted had findings related to Durable Medical Equipment (DME) prescriptions and refills for incontinence supplies.
Special attention should be taken to review the prescription/order section of the DME policy manual.
All prescriptions/orders must include the following elements:
- Member name and date of birth.
- Date the prescription was written.
- Quantity and length of need, such as six daily for one year (as needed is not valid).
- Valid diagnosis code for the need of the supply.
- The RX must be signed and dated by prescribing practitioner.
Along with a valid RX, the following are also required for any DME refillable single-use item:
- Some type of communication log which records the date and name of person requesting a refill.
- How many individual supplies are on hand.
- An invoice if the supplies are delivered or shipped.
- Signed receipt of delivery or pick-up by the member or designee must be legible with the relationship of the designee to the member.
- Delivery records must contain the number of items. For example, Manufacturer A packages small-sized briefs in lots of 20 and Manufacturer B packages small- sized briefs in lots of 18. This will assist in validating the number of “units” billed to ND Medicaid.
Providers may submit a service authorization for quantities over the monthly limit if needed.
Service authorizations must have an updated prescription and physician visit note. The monthly limit for A4520 (incontinence garment) was increased to 200 in May 2023 to assist in these scenarios so requesting over the monthly limit will be the exception rather than the norm. The limit for A4554 (disposable under pads) remains 70 per month.
For more information, refer to the quick reference policies.
State Form (SFN) updates

Several forms have been reviewed and updated. Please use the most recent version of the form.
ND Health Service Corps Loan Repayment Program 
The Primary Care Office in North Dakota Health and Human Services (ND HHS) is encouraging new graduates and established health care professionals to apply for the 2024 North Dakota Health Service Corps Loan Repayment Program by March 31, 2024. The North Dakota Health Service Corps comprises four statewide support-for-service programs that provide financial support to participating health care providers who work in/with underserved communities and populations.
ND HHS reminds health care professionals who have honed their skills and talents here “at home” that promising careers in health care exist in North Dakota. North Dakota can assist with loan repayment opportunities for qualifying health care professionals. Learn more about our campaign: Love you to stay.
Who is eligible?
Professions eligible for these support-for-service programs include physicians, nurse practitioners; physician assistants; registered nurses and pharmacists. Eligible behavioral health professions that also qualify include clinical psychologists, licensed addiction counselors, licensed professional counselors, licensed social workers, registered nurses and behavioral analysts. Please refer to each individual loan repayment program for more information on the eligible disciplines and qualifications.
How to apply?
Visit the North Dakota Primary Care Office webpage for information on loan repayment programs, qualifications, and application requirements. The application period runs from January 15 to March 31, 2024.
Who to contact?
If you have questions, please reach out to Kalee Werner, director of the Primary Care Office.
Report changes in ownership within 35 Days (Provider Enrollment)

All changes in ownership (both direct and indirect ownership) are required to be reported within 35 days of the change.
Providers enrolled in both Medicare and ND Medicaid must update ownership in both your Medicare and ND Medicaid records. Medicaid applications may be delayed until the Medicare record has been updated.
Here's how to report changes in ownership. Submit:
- A statement of whether the business NPI and/or Tax ID has changed.
- Old owner(s) first and last name(s) and termination date(s) (if applicable).
- New SFN 1168. Read instructions before completing.
- Effective date of change.
- Name and contact information of person sending the request. Note: the reporting person must be listed in your record as an authorized representative, managing employee, board member or owner.
- Please contact your organization administrator to ensure the reporting person appears in one of these categories in the web portal prior to submitting your request.
- If you need to add the reporting person to the record, please have the organization administrator add them as an authorized representative and submit an updated SFN 1168.
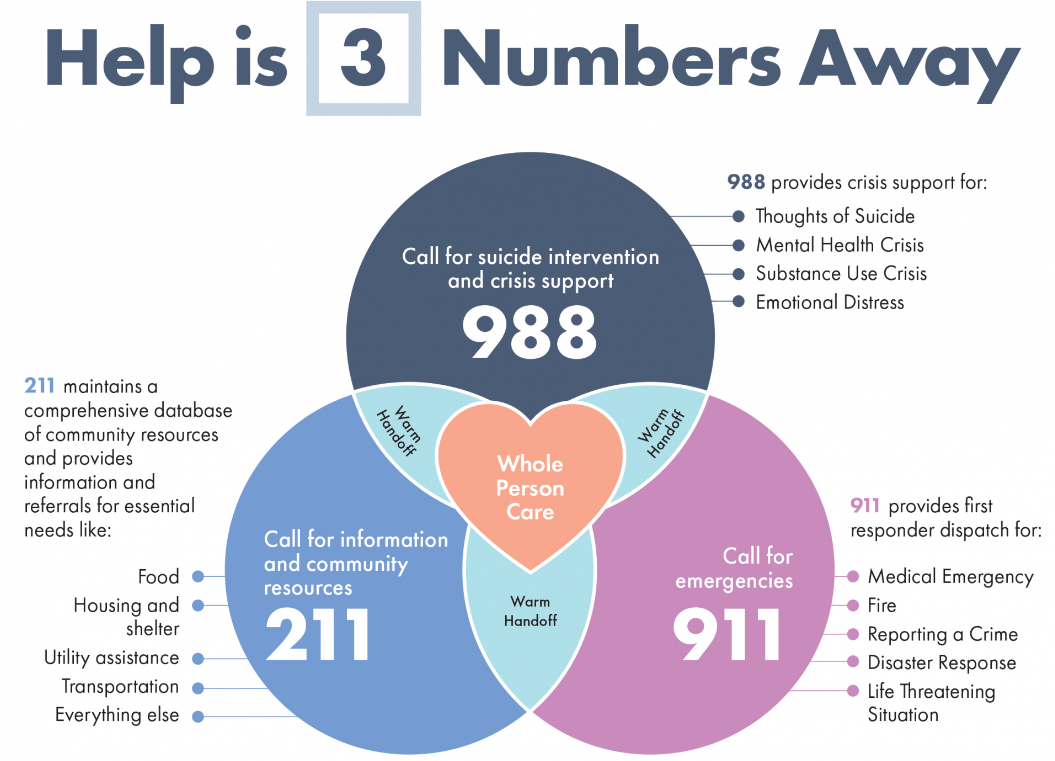
Learn more about the 988 Suicide and Crisis Lifeline.
Stay in the know! Medicaid provider newsletter subscription

Signing up to receive ND Medicaid’s quarterly provider newsletters is easy.
Step 1: Go to the Provider webpage.
Step 2: Enter your email address and click submit.
Step 3: Follow directions to set up and choose your subscription options. Select Medicaid Provider Newsletter.