This page contains additional information presented by a team from the Life Skills and Transition Center, Grafton, N.D. at the American Association on Intellectual and Developmental Disabilities national conference.
2024 Conference - Louisville, KY
Trends in Competency to Stand Trial, Criminal Responsibility and Culpability Evaluations for People with I/DD
Range | Mean | Median | Mode | |
| Number of charges | 1-5 | 1.9 | 1 | 1 |
| CAST-ID Total | 14-49 | 34 | 35 | 30 |
| Georgia | 20-96 | 62 | 60 | 46 |
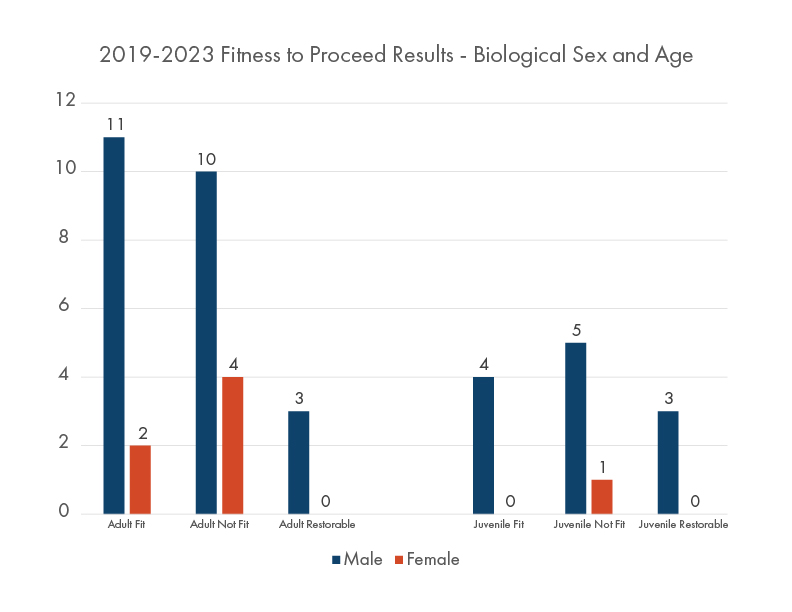
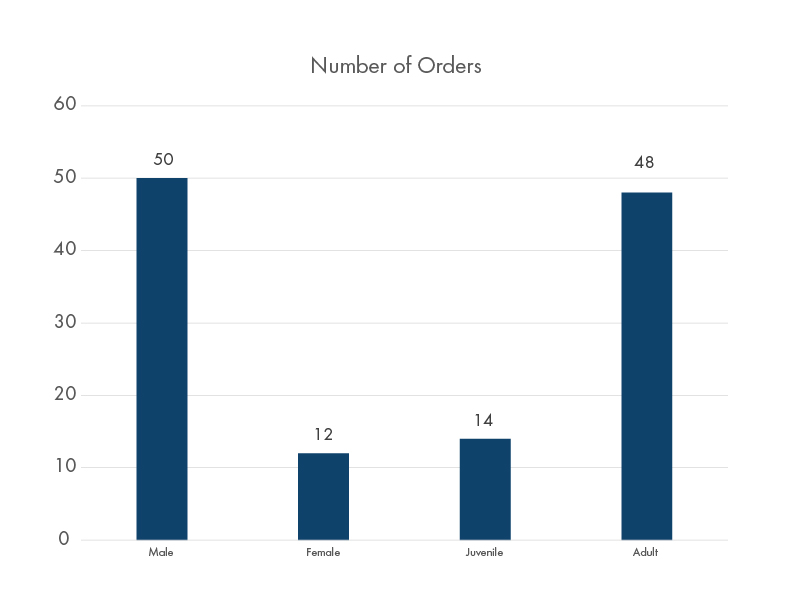
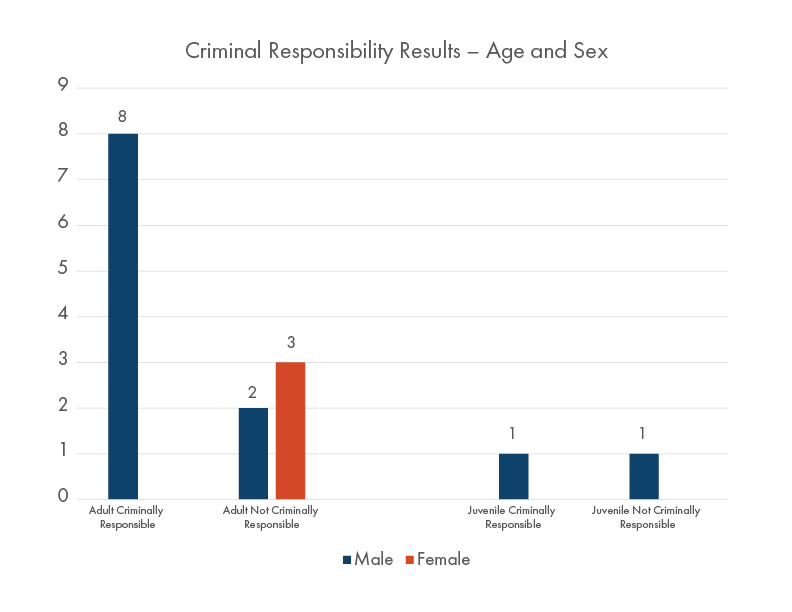
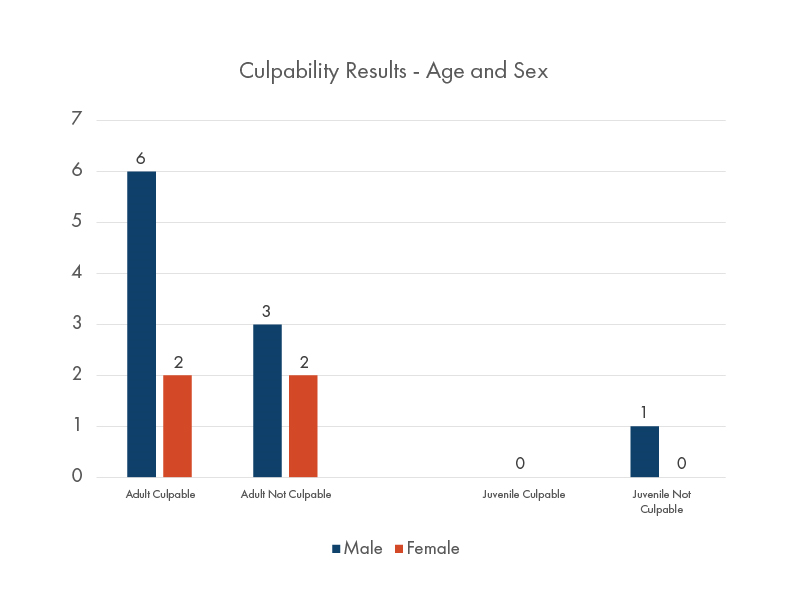
- Adult and juvenile males are more likely to be referred than females
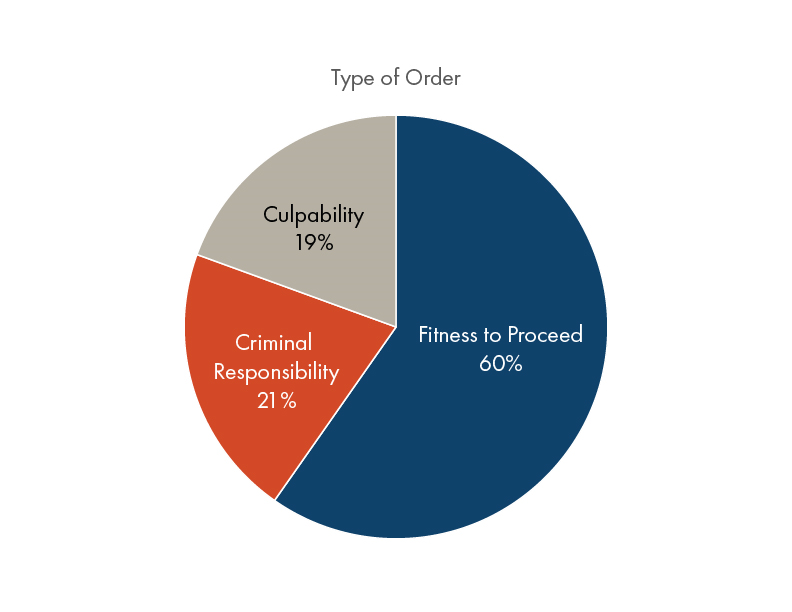
- The most common orders are competency to stand trial evaluations
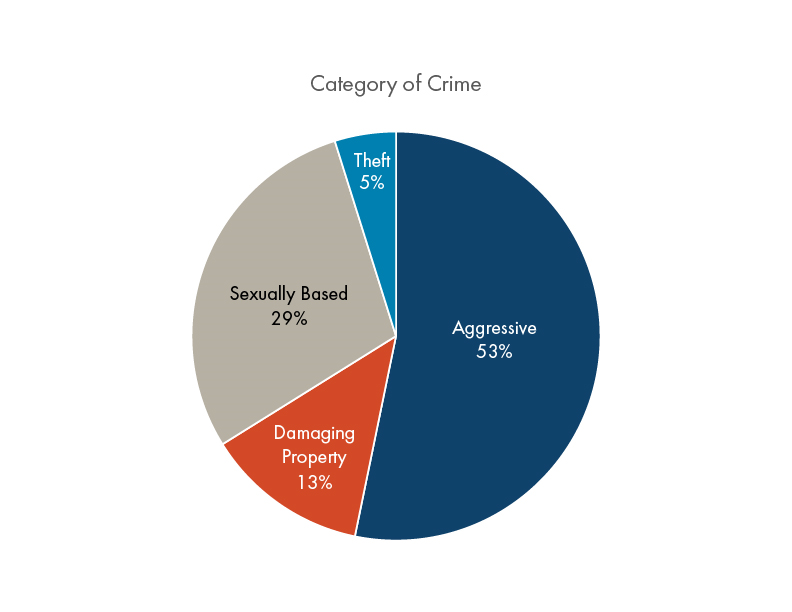
- Over 2/3 of index crimes involve physical or sexual violence
2023 Conference - Pittsburgh, PA
Effective Crisis Support in a Geographically Large Rural State
Accessing Crisis Services
The first step to accessing statewide crisis stabilization services in a non-emergency situation is to hold a meeting with all community team members.
After guardian consent is obtained, the Developmental Disability Program Manager will contact the Transition and Diversion Coordinator to initiate crisis stabilization services.
The CARES manager will arrange for an initial consultation between the community-based team and relevant LSTC professional disciplines; i.e., psychology, speech, etc. The type and frequency of supports and assessments is determined and documented in a formal action plan. On-going meetings to discuss progress and need of continuing services are scheduled as appropriate. Once a period of stability has been established, supports will be gradually faded and the case will be closed. At anytime, the case can be reopened.
Available supports include:
- On-site direct support professional assistance,
- Observations and training,
- Behavioral health services, and
- Access to experts in the field of psychology, behavior analysis, social work, occupational therapy, physical therapy, speech therapy, nursing, pharmacy, adaptive equipment, and nutrition.
Process
- Team Meeting
- Contact Diversion & Transition Coordinator
- Initial Consultation & Action Plan Development
- Service Delivery
- Fading and Case Closure
Crisis Stabilization Barriers and Future Goals
Barriers to Fully Implementing Statewide Crisis System
- People with complex behavioral or medical needs can overwhelm the private provider system.
- Shortage of licensed I/DD providers serving youth.
- Statewide shortage of Direct Support Professionals.
- Current population at LSTC limits the allocation of resources for crisis stabilization.
Short-term Goal
- Reduce LSTC census to reallocate resources for crisis admissions and stabilization.
- Expand access to and utilization of statewide crisis stabilization and prevention services.
Long-term Goals
- Advocate for funding that matches the current need for state level services.
- No long-term admissions (more than one year) to the LSTC.
- Partner with psychiatric residential treatment facilities (PRTFs) to increase their capacity to serve youth with I/DD and behavioral health conditions.
- Partner with Children and Family Services Section to increase the capacity for youth with I/DD and behavioral health conditions being placed in foster care vs. institutionalization.
- Collaborate with licensed residential I/DD providers for an increase in services for youth.
Definition of Roles
Behavioral Health
- Licensed psychologists and applied behavior analysts with 100+ years of specialized experience assessing and treating people with I/DD
Crisis Stabilization Coordinators
- Professionals who support people with I/DD in crisis by working directly with families, providers, and community partners.
Multidisciplinary Team
- Team of specialized experts in the fields of psychology, behavior analysis, social work, occupational therapy, physical therapy, speech therapy, nursing, pharmacy, adaptive equipment, and direct support professionals.
Adaptive Equipment Services
- Specialists who make customized equipment for people with disabilities across the state.
CARES Outpatient Clinic
- Speech, occupational, and physical therapy services in an outpatient clinic setting in Grafton, ND.
Who we are: A specialized team providing transition and diversion support for people in crisis to ensure opportunities to live in communities of their choice.
Transition: Services provided to support peoples’ return to communities of their choice. Planning for return begins the day of admission to LSTC and services extend to 30 days post discharge.
Diversion: Services provided to support people to remain in their homes while avoiding extended psychiatric hospitalization or institutionalization.
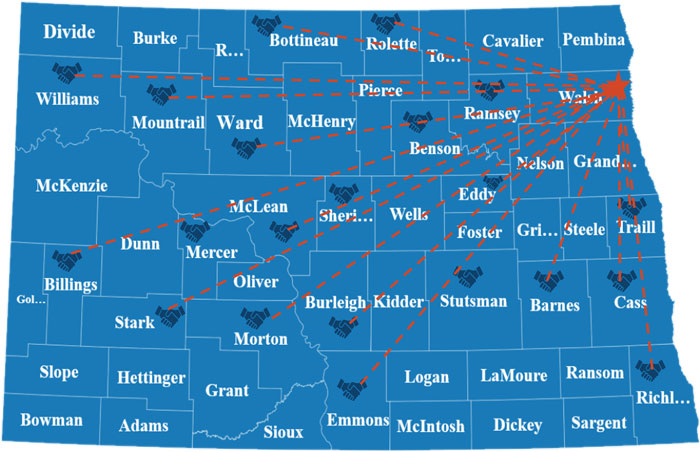
Life Skills and Transition Center provided transition support and crisis stabilization to 129 people in 21 counties between July 2021 – Dec 2022.
Available Crisis Stabilization and Prevention Services
Family Supports
- Home Assessment
- Crisis Support
- Outreach
- Child & Parent Training
- Team Meetings
- Check-ins
Agency Supports
- Training
- Resource Development
Citizen Supports
- On-site Assessment
- Crisis Support
- Skills Training
- Training on Person
- Team Membership
- Check-Ins
- Telehealth
Community Outreach
- Training
- Coaching
- Consultation
Generic Crisis Supports
- Support in Crisis Settings
On-site Support
- All Ages
- On-going Support Based on Need
Crisis Services Data - Applications for Services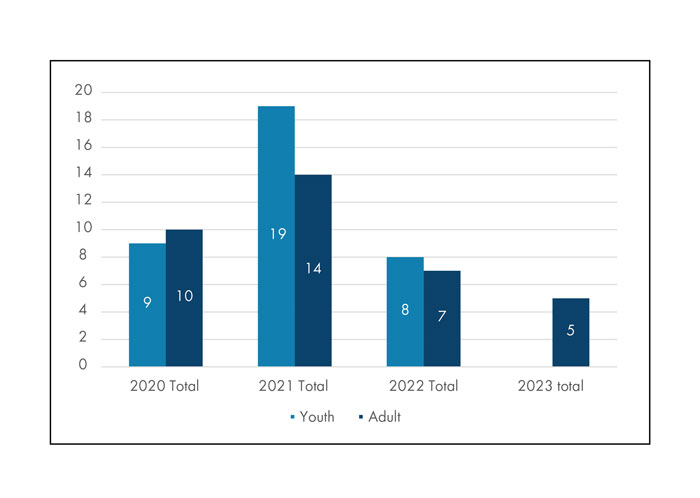
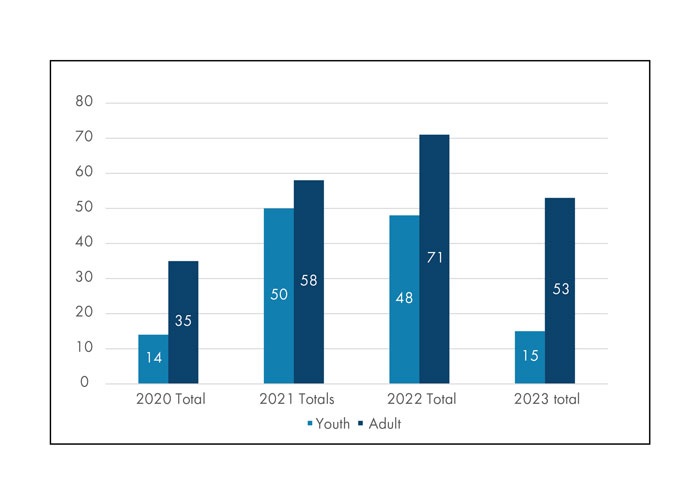
Application for services peaked in 2021. While applications are down, service delivery has increased.
*Access to services has been streamlined to reduce paperwork and quicken response time.
Crisis Services Data - Follow-Up Consultations
Consultations have increased annually since 2020.
2023 is on track to have 159 adult consults (highest number) and 45 youth consults (second year in decline).
Interventions for Systems Barriers
Barrier Example #1:
Person does not accept support from their provider or legal decision maker. Provider is not willing to continue serving the person. Person ends up “stuck” at psychiatric hospitals with no where to go.
Interventions:
- Work with the I/DD system to identify possible residential settings in a new community for a fresh start.
- Brainstorm with I/DD system and providers on nontraditional delivery of supports.
- Weekly visits with designated team member to provide a lifeline for service delivery.
- Negotiate with the person on the type, frequency, and method of service delivery.
- Implement “harm reduction” strategies.
- Regular check-ins when person chooses unsafe living conditions.
- Provide access to medical assessment, treatment, and interventions for high-risk behavior without judgment.
- Build rapport in an effort to encourage less risky activities; i.e., using marijuana instead of meth or using safer sex practices.
Barrier Example #2:
Polices & Practices surrounding discharge from private providers are inconsistently implement by private providers and do not always represent the best interest of the person served.
Interventions:
- Brainstorm with I/DD division to develop more robust discharge policies and practices.
- Collaborate with NDACP for ideas to prevent discharges in general and to ensure that policies and practices are followed.
- Identify and address barriers to requesting and accepting support before the situation rises to the level of a potential discharge.
Barrier Example #3:
Legally appointed decision makers ask to be removed with no replacement option, despite the continued need for this service. Additionally, there remains a lengthy waiting list for people who need a legally appointed decision maker.
Interventions:
- Support legal decision makers in challenging situations.
- Provide education on other options available other than rescinding.
- Ensure that parents and families are provided education about the process, cost, and need for petitioning for guardianship at least one year prior to their loved one turning 18.
Interventions for Agency Barriers
Barrier Example #1:
Private providers request and access behavioral health and crisis services with no intention of utilizing them in order to fulfill state discharge requirements.
Interventions:
- Provide outreach education about the benefits of accessing services as a preventative measure rather than waiting until it reaches the point of crisis or possible discharge.
- Build rapport and consultative readiness relationships with agencies who are less familiar with available resources and services.
- Reach out to agencies who have possibly had less than ideal experiences with crisis/behavioral health services.
Barrier Example #2:
Private providers use emergency rooms and psychiatric hospitals as methods of circumventing the 30-day discharge requirements. People with disabilities are sometimes brought to the emergency room to access psychiatric hospitalization and the provider then discharges the person from their services. The person then has lost their home and has no where to go.
Interventions:
- Work with provider to rescind 30-day discharge notice and identify the barrier(s) to continuation of services.
- Offer on-site crisis support, coaching, and modeling.
- Offer behavioral health services to develop methods of positive support plans to address any behavioral health concerns.
Interventions for Family/Guardian Barriers
Barrier Example #1:
Family does not consent to recommended treatment, medications, or assessments deemed necessary by professionals.
Interventions:
- Build rapport with the family by validating concerns and the family’s desire for the best outcomes for the person. Identify the family’s concerns and attempt to address them through education and brainstorming.
- Emphasis the benefits of the recommendations.
- Encourage connecting to other families in similar situations.
- Require signed documentation of choice to withhold consent to recommended treatments and assessments. Include a detailed description of the associated risks of that choice that are specific to the situation; i.e., exacerbation of mental health symptoms, possible hospitalization, impairment in social relationships, etc.
- If lack of consent is likely to cause harm to the person, interferes with daily life, or places the person’s ability to stay in their home at risk, report the situation to Protection & Advocacy.
Barrier Example #2:
Family is hesitant or choosing not to access services, even though loved one is in crisis. Family may choose not to let support professionals in the home, may miss appointments, or may not follow through with recommendations.
Interventions:
- Build rapport and facilitate an open discussion about the reasons for the hesitation. Is the family afraid of having outside people in the home?
- Validate hesitancy, fears, and concerns.
- Educate on the benefits of accepting services.
- Start with small goals. Work with the team to identify what service/support the family is most likely to accept. Once a pattern of acceptance for that support is established, add additional services.
- If lack of consent is likely to cause harm to the person report the situation to Protection & Advocacy.
Interventions for Person-Served Barriers
Barrier #1
Person does not want to receive supports and/or does not think supports are necessary. This places the person at risk of harm and negative outcomes.
Interventions:
- Collaborate with the team to designate someone specific to build rapport and trust with the person.
- Educate the person on the benefits of services; i.e., how can services help them meet their goals? How can the person “use” services for their benefit.
- Implement “harm reduction” strategies.
- Regular check-ins when person chooses unsafe living conditions.
- Provide access to medical assessment, treatment, and interventions for high-risk behavior without judgment.
- Build rapport in an effort to encourage less risky activities; i.e., using marijuana instead of meth or using safer sex practices.
- Start with small goals. Work with the team to identify what service/support that the person is most likely to accept. Once a pattern of acceptance for that support is established, add additional services.
Patterns of Institutionalization of Youth with Intellectual and Developmental Disabilities in ND
Youth Transition Services Data
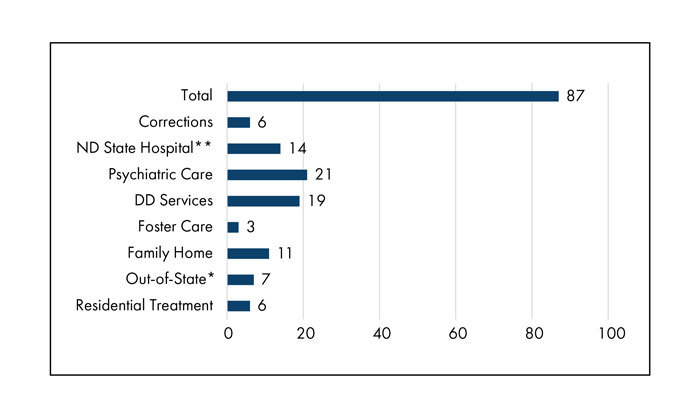
The majority of youth (35) come from inpatient hospitalization. This reflects the need to revise discharge policies and increase availability of out of home, intermediate care for youth.
Minors are no longer being admitted to the ND State Hospital. Youth with I/DD are no longer being sent out of state.
*Out of state: last youth came in February 2018
**ND State Hospital: last admission came in June 2012
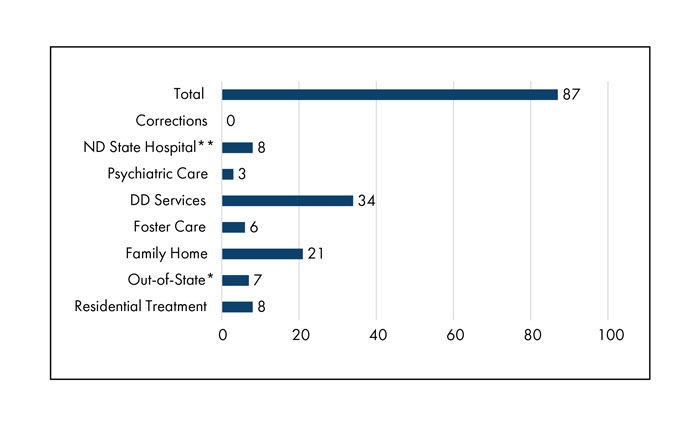
The majority of the youth (34) were living in I/DD service settings prior to admission.
Minors are no longer being admitted to the ND State Hospital. Youth with I/DD are no longer being sent out of state.
*Out of state: last youth came in February 2018
**ND State Hospital: last admission came in June 2012
Youth Services in North Dakota
- The majority of youth admitted to the LSTC are 12 years or older.
- There are currently 37 residential providers of I/DD services in ND and only 7 serve youth.
- 796 youth between ages 12-20 currently receive some sort of I/DD services.
Definitions of Youth Service Placement Options
Residential Treatment
- Psychiatric Residential Treatment Facilities (PRTF)
I/DD Services
- Typical ICF homes & HCBS settings
Family/Foster Home
- Living in typical family home or foster setting with or without in home support services
Psychiatric Hospital
- Generic, private psychiatric hospitals
State Hospital
- Extended hospitalizations for people aged 18+ who are experiencing crisis
- Historically included those aged 12+
- Sometimes people aren’t discharged because there is no where to go
Out of State
- Residential treatment settings located in other states
Stop Walking on Eggshells: Supporting People with I/DD and Borderline Personality Disorder
Splitting
- Splitting happens when different people in the support network disagree over how to interact with the person, often to an extreme degree.
- This often results in some team members being labeled in a positive light, “good” and the rest in negative one, “bad.”
- This frequently leads to ineffective communication and interferes with treatment. It also negatively impacts team members motivation to provide services.
- Splitting can be initiated by the person, family, or any team member.
Triangulation
Triangulation occurs when one member of the team sides with another member to blame the rest, often to gain or keep control, deflect responsibility or avoid acceptance of the situation.
For example, the school may “pair” with the family to blame the residential team for problems that are occurring. Another example is the family pairing with their loved over medical recommendations the person does not want. The team is blamed for the recommendation.
Team - Family - Person
Functions of effective treatment of Borderline Personality Disorder (Linehan, 1993)
Enhancing Person-Served Capabilities (Linehan, 1993)
Learning new skills is imperative. Teaching these skills can be done in a variety of ways. Options include offering group or individual skills training or writing formal learning objectives that are imbedded into the person’s support plan. The exact skills needed are identified through an assessment of the functions of the target symptoms and the person’s short- and long-term goals.
Ensuring Generalization (Linehan, 1993)
It is not enough for the people we support to learn or know skills or to even use those skills in some situations. They must be able to use those skills across all environments and all people. Skill generalization is often much more challenging that skill acquisition. Specific guidelines for coaching and supporting skill use should be documented in the ecological and positive programming sections of the MPS. It is critical that all team members reinforce skill use.
Direct support professionals (DSPs) are an essential part of this process. DSPs spend the most time with the people we support, affording them the perfect opportunities to coach people on skill use throughout their day.
Enhancing Team Member Capabilities and Motivations (Linehan, 1993)
Working with people who have Borderline Personality Disorder (BPD) can be exhausting and burn out is common. When people are burnt out, or at their limit, it is almost impossible to provide effective treatment. You may say or do things that are not helpful to the person; i.e.; lashing out, not following plans, etc.
Staff meetings and administrative team reviews can provide support for those working with BPD.
Enhancing Motivation of Person Served
Successful treatment requires that we increase the person’s willingness and motivation to try new skills in new situations AND to agree to give up old, maladaptive patterns of behavior.
This is accomplished by building rapport with the person, the reinforcement strategies in the methods of positive support plan (MPS), praise for using skills, and in vivo coaching from DSPs during day-to-day activities.
Tips when working with Borderline Personality Disorder (Linehan, 1993)
Leave if necessary
- If the person is upset with you, leave the situation if it is safe to do so. Switch out with another DSP, if possible. If you find yourself becoming upset, it is best to remove yourself from situation. Offer to find another team member for the person to talk to.
Separate the person from the behavior
- Remind yourself that the person is not the problem, their actions are. Try not to take it personally. People with this disorder tend to lash out at those around them. It most likely has nothing to do with you.
Address feelings before facts
- Focus on feelings rather than words. People with this disorder can sometimes make extreme emotional statements, such as “I hate Angela. . . I’m going to kill myself. . . or no one is helping me.” Do not try to argue with the person about these statements; rather, address the underlying emotion. Examples, “you are pretty angry with Angela right now. . . it sounds like you are feeling hopeless. . .you feel like you’re not getting the help you need.”
Clarify the situation
- It’s not uncommon for a person with BPD to come to you in an extreme state of emotional dysregulation. At this point, the best thing to usually do is ask the person to help you understand the situation. This likely involves assisting the person to calm enough to communicate the specific details. Once you have a relatively clear idea of what happened, you can then use validation strategies (feelings before facts).
Delay and Distract
- If the person continues to be emotionally dysregulated after validation, try to distract or delay the person. Delaying a response allows time for the person’s emotions to decrease and lessens the chance of impulsive, risky behavior.
BPD Recommended Resources
- The Emotional Regulation Skills Systems for Cognitively Challenged Clients: A DBT Informed Approach (2016) - Julie F. Brown
- DBT Skills Training Manual - Marsha M. Linehan
Target Symptom Hierarchy Examples
Safety Interfering Symptoms
- Self-injury, (contagion effect of other’s actions), physical aggression, property destruction, any other action that puts someone at risk of harm
Treatment Interfering Symptoms
- Choosing not take or complete medications/treatments, verbal aggression, lying, false accusations, missed appointments, anything else that interferes with delivering effective treatment
Quality of Life Interfering Symptoms
- Somatic symptoms, inadequate grooming, not following schedule, anything else that interferes with a person’s quality of life
Skills to Increase
- Accurate communication, coping skills, relationship skills, self-management of somatic symptoms, vocational skills, activities of daily living, any replacement skill needed or identified in a functional assessment
When designing treatment plans using dialectical behavior therapy principles and positive behavior supports, it is essential to know which symptoms to target first. Any action that interferes with a person’s safety should always be prioritized first in order to maximize the likelihood of successful treatment and avoiding hospitalization and/or institutionalization.
Once safety interfering symptoms have been extinguished, the focus shifts to actions that interfere with the person benefitting from treatment OR team members willingness to provide treatment.
Work can then begin on those actions that interfere with a person’s quality life. This often goes hand in hand with teaching new skills.
There's Something Wrong With Me! Managing Frequent Somatic Complaints While Avoiding Unnecessary Clinic Visits, Use of ER and Hospitalizations
Ingestion of Foreign Bodies Protocol
Protocol for Responding to Ingestion of Foreign Bodies
1. Person reports having ingested a foreign body. Examples include batteries, screws, pens, bottle caps, tacks, mulch, rocks, etc.
2. Person supported is sent to closest clinic as soon as possible (usually with a DSP and a nurse) for an x-ray to confirm something was swallowed.
- The agency nurse (or supervisor) should call ahead to the clinic to explain the situation and the desired response from the clinic team. This typically includes:
- Minimal interaction with medical staff
- Share minimal required follow-up information
- Admission only if absolutely necessary
3. After assessments are complete, bring the person home and wait for recommendations (if possible and medically appropriate).
- Common interventions experienced by the LSTC team include
- Letting the item pass with the assistance of bowel meds
- Removal per medical recommendation (commonly with an upper or lower scope).
4. Team members not at the clinic will prepare for crisis management if the person’s desired procedure isn’t prescribed.
- This might involve:
- Increased staffing ratio
- Removal of dangerous items
Who Stole My Rights? Using Experienced Based Learning Activities to Teach Rights and Responsibilities and Advocating for Rights Restoration in a CQL Accredited State-Run Institution
Personalized Rights Books
- Each person living at the LSTC has a personalized rights book.
- The book is formatted to meet the person’s unique abilities, utilizing pictures, technology, and other adaptations.
- Each book should be readily accessible.
- Rights that are most important to the person are highlighted, based on CQL personal outcome interviews.
- Includes information about their legally appointed decision maker (if there is one) and specific details from the guardianship order.
- Information on the corresponding responsibility is highlighted.
- It is reviewed by the team annually and updated as needed.
Examples:
I have the RIGHT to . . .
- Receive mail at my home
- Get support with my mail
- Open my own mail
- Keep my mail private
My RESPONSIBILITY is . . .
- Ask for help if I need it
- Report concerns
- Keep my address private
- Keep information safe
I have the RIGHT to . . .
- Carry my own money
- Access my money
- Spend my money
- Get help with budgeting
My RESPONSIBILITY is . . .
- Follow my budget
- Pay my bills
I have the RIGHT to . . .
- Choose where I live
- Choose who I live with
- Who comes to my home
- When people can visit
My RESPONSIBILITY is . . .
- Pay the bills
- Keep my home clean
- Maintain my home
I have the RIGHT to . . .
- Learn job requirements
- Pick which jobs to apply for
- Say no to a job
- Accept a job
My RESPONSIBILITY is . . .
- Go to work
- Follow work rules
- Be on time
- Get job training
Center Concerns Form
Center Concerns Forum is a monthly gathering for people living at the LSTC and their direct support professionals. It is hosted by the social work department and quality support services. People can participate in person or virtually. Focus points include:
- Rights education
- Agency changes and goals
- Recognition of peoples’ successes
- Opportunities to voice ideas for agency improvements
Legislative Group
Legislative Group meets weekly during North Dakota’s legislative session. It is hosted collaboratively between LSTC’s clinical services department and Protection and Advocacy. It focuses on:
- Educating people on the government process
- Tracking relevant disability and mental health bills
- Voter education
Rights Carnival
Rights Carnivals are held monthly for the people living at the LSTC. Each carnival features a different right and provides three interactive activities designed to educate on that right and corresponding responsibility.
- Rights and responsibilities
- Opportunity for peer education
- Fun way to learn

Rights Education Game Shows
When using game shows, it is best to have options for people served to be paired with direct support professionals or a peer as well as an option to participate individually. Each person or pair is given a marker board so that everyone has a chance to answer the question. Make sure the content of the game is relevant to the people participating, have prizes, and keep it short.
Ask - Act - Advocate - Educate - Experience - Exposure
People living at the LSTC are provided with training designed to help them learn how to make informed choices. Informed choice improves quality of life and associated outcomes.
The LSTC uses two specific training models from CQL to teach about informed choice:
- Ask – Act – Advocate
- Educate – Experience – Exposure
When is Enough, Enough? Addressing Treatment Interfering Behavior by Parents and Legally Appointed Decision Makers in a CQL Accredited State-Run Institution
Medical
Treatment Interfering Behavior #1: Family/guardian requests the use non-evidenced based treatments, multiple non 3rd party tested supplements, dismissal of standard western medicine, and/or restrictive meal plans.
Interventions:
- Risk Mitigation: If the person is able, encourage and support them to communicate their thoughts on the recommended treatment/meal plan/supplements. If necessary, consult with Protection and Advocacy about legal limitations of guardian choice in non-traditional treatments.
- Educate: Agencies may provide gentle education about the possible interactions between various supplements and western medications. Teach self-advocacy skills and support the person to advocate if they disagree with their guardian.
- Policies: Agencies may consider adopting policy where the agency will not administer non 3rd party tested supplements. Policies should clearly outline who will write supplement orders, agency financial limitations, and clearly define what is covered in “cost of care” in an ICF setting.
Treatment Interfering Behavior #2: Family/Guardian withholds consent from recommended treatments/assessments or provides passive consent “under duress.”
Interventions:
- Risk Mitigation: If necessary, consult with Protection and Advocacy about risk from harm for withholding consent. The agency may need to advocate for guardianship changes.
- Educate: Provide the guardian with a detailed document outlining the possible risks and benefits of both withholding and giving consent to the recommend intervention. Educate guardians that consenting under duress is not legal consent.
- Policies: Agencies may consider develop a policy that requires the guardian to sign a document indicating they understand the risks of withholding consent.
Presumed Incompetence
Treatment Interfering Behavior #1: Family/Guardian tries to control every aspect of the person’s life (finances, activity choice, personal expression, food, etc.) limiting self-determination and choice.
Interventions:
- Risk Mitigation: Build in natural opportunities for choice throughout the person’s day and document person’s reaction and participation in the chosen activity.
- Educate: Provide education on the right to personal choice. Provide education on the benefits of learning how to make an informed choice and how that impacts quality of life. Teach self-advocacy skills and support the person to advocate if they disagree with their guardian.
- Policies: Develop agency policies that clearly outline what the agency views as “overreach” with regards to personal choice.
Treatment Interfering Behavior #2: Family/guardian insists on supports that are assessed as being overly protective.
Interventions:
- Risk Mitigation: Contact Protection and Advocacy if all other interventions are ineffective.
- Educate: Provide education on the fading process of rights restrictions. Provide education on the role of the Human Rights Committee and the necessity of their approval to implement rights restrictions.
- Policies: Develop agency policies that clearly define the fading process for all rights restrictions.
Treatment Interfering Behavior #3: Family/guardian withholds consent for discharge referral.
Interventions:
- Risk Mitigation: Provide opportunities for the person to visit other living situations.
- Educate: Provide education about the possible benefits of moving to a less restrictive setting. Educate about the supports and services available. Provide education on the Olmstead Act. Assist in setting up tours and meetings with possible providers. Teach self-advocacy skills and support the person to advocate if they wish to move.
- Policies: Consider developing policies that require referral to community providers.
Hostility
Treatment Interfering Behavior #1: Family/guardian engages in splitting and triangulation.
Interventions:
- Risk Mitigation: Require all team members to participate in team meetings to decrease opportunities for splitting. Appoint an administrator to provide mediation during team meetings in order to keep the proceedings civil. Focus on facts, not interpretations or feelings. Begin each meeting with a reminder that we all have the same goal, which is helping the person live their best life as they choose. Thorough documentation of all conversations and meetings. Use a third-party witness, if needed.
- Educate: Provide education on the team process and team roles as well as realistic limitations of services. Offer information on other resources available. Remind family/guardian of availability of Protection & Advocacy. Educate family/guardian on the effects of splitting/triangulation on the person served and the willingness of agencies to provide services.
- Policies: Develop a formal process for families/guardians to report a concern or grievance. Develop policies that define team member roles and responsibilities as well as communication expectations.
Treatment Interfering Behavior #2: Family/guardian using verbal aggression or makes threats towards the agency or specific team members.
Interventions:
- Risk Mitigation: Identify the inappropriate communication and communicate that if it does not immediately stop, the meeting/call will end. Set boundaries at the beginning of the meeting or call. Appoint a non-team member to provide mediation during team meetings in order to keep the proceedings civil. Focus on facts, not interpretations or feelings. Use a third-party witness in all further communication, if needed.
- Educate: Educate family/guardian on the effects of this behavior on the willingness of agencies to provide services.
- Policies: Include these incidents in official reports to the agency in order to develop risk mitigation. Develop a formal process for families/guardians to report a concern or grievance. Develop policies that define team member roles and responsibilities as well as communication expectations.
Abuse, Neglect and Exploitation
Treatment Interfering Behavior #1: Family/Guardian steals the person’s medication.
Interventions:
- Risk Mitigation: No longer give that family member access to or control of the medication. Assign an alternative person as being responsible for the medication. Report the incident to appropriate agencies. Consider providing support during visitation. Require signing form when accepting and returning medications.
- Educate: Provide education on the agency’s response to any mishandling of the medication.
- Policies: Develop policies regarding agency’s response to mishandling of medication.
Treatment Interfering Behavior #2: Family/guardian fails to follow team approved supports.
Interventions:
- Risk Mitigation: Immediately intervene to avoid harm. Address the concern with the family/guardian as soon as it is discovered. Report the concern to the appropriate agency, such as Protection and Advocacy.
- Educate: Educate the family/guardian on the importance of the support and the possible harm that could come from not implementing it.
- Policies: Ensure there are policies regarding abuse, neglect, and exploitation as well as mandatory reporting guidelines.
Treatment Interfering Behavior #3: Family members/co-guardians disagree on treatment decisions
Interventions:
- Risk Mitigation: Ask family to designate a point person. Ask family to work out disagreements outside of the team process, come to a consensus, and then communicate final decision to the team. Involve Protection and Advocacy if needed.
- Educate: Provide education on the legalities of multiple guardians based on the specifics of the court order.
- Policies: Develop policies regarding working with people who have multiple guardians.
Treatment Interfering Behavior #4: Family/guardian appears to be overly focused on the person’s weight and/or engages in “body shaming.”
Interventions:
- Risk Mitigation: If the person is able, encourage and support them to communicate their thoughts and feelings about their weight. If necessary, consult with Protection and Advocacy about legal limitations of guardian choice in weight.
- Educate: Teach self-advocacy skills and support the person to advocate if they disagree with their guardian. Educate the family/guardian on the effects of their behavior on the person’s mental health. Educate on healthy weight ranges and realistic weight goals.
- Policies: Ensure there are policies regarding abuse, neglect, and exploitation as well as mandatory reporting guidelines.
Treatment Interfering Behavior #5: Family/guardian does not give or respect the person’s need for personal privacy in their own bedroom/bathroom.
Interventions:
- Risk Mitigation: Immediately intervene and ask the family/guardian to give the person privacy and then address the issue in more detail. Identify specific places for visitations. Consult with Protection and advocacy if needed.
- Educate: Educate on the importance of privacy for every person as well as on healthy boundaries between adult family members.
- Policies: Develop family/guardian visitation guidelines. Develop policy outline procedures for intervening in these situations.
Restoring Rights and Advocating Guardianship Changes in a CQL Accredited State-Run Institution
Restoration Plans
Restoration plans are formal documents outlining each right that is restricted as well as the specific details included in guardianship orders, if applicable. The plans are developed by the team, updated as needed, and are approved by the Human Rights Committee at least once a year.
Restoration Plan Example: Access to Money and Rep Payee
Description: Agency is Rep Payee for Glen’s money.
Rationale: Glen is vulnerable to financial exploitation.
Potential risks if not utilized: Glen is worried he would spend too much money, not budget well, or over-draft. Glen feels he would help others who need money. He may lose his benefits.
Potential risks from the support being implemented: Glen states he is okay with his rep payee. Glen may not have immediate access to his money as he needs guardianship and agency approval for more than $150.00.
Restoration Plan: Glen helps with his finances, but needs assistance to pay his bills. When asked if he would like to do more with his finances, he states "I can't write."
Support/Objective: Using a price sheet, Glen will enter the correct amount for clothing items into the till. Glen is supported to utilize the Quicken program to keep track of his finances. Glen is supported to count back change to customers when at work
Restoration Plan Example: Locked Sharps
Description: Knives are locked in kitchen.
Rationale: Andy needs support to use knives safely.
Potential risks if not utilized: Andy struggles staying focused and controlling his impulses, putting him at risk of cutting himself. He lives with others who use it as a weapon.
Potential risks from the support being implemented: Andy may display aggression if he is asked to wait.
Restoration Plan: Staff support Andy to learn to cook and use utensils safely (cutting away from his body, not carrying the knife from place to place, putting it down when not using, watching for fingers and hands being out of the way, being calm and feeling safe before using these utensils).
Support/Objective: S4. Andy will be supported to become independent with his activities of daily living. S7. Andy will be supported to utilize knives and kitchen equipment safely during meal preparation.
Restoration Plan Example: Locked Sharps
Description: Parent controls placed on personal phone, disabling of camera on phone, blocking receipt of pictures and videos.
Rationale: John recently acknowledged sending nude photos of himself to others. He has demonstrated adequate knowledge of internet safety but does not consistently apply this knowledge.
Potential risks if not utilized: John may face legal charges if he sends nude pictures unsolicited to adults or if he sends pictures, solicited or not, from minors. The person receiving the photo would have control over it and my use it in a way that John does not agree with.
Potential risks from the support being implemented: John loses some independence in using all features of his phone, he may lose out on opportunities to receive appropriate pictures from friends and relatives. John expressed that he currently is OK with these restrictions.
Restoration Plan: John will be supported to purchase adult media. After 2 months from the purchasing, fading will begin. Each step will involve 3 months of success. Step 1) Enable the camera and do a phone check once daily at a random time. Step 2) Phone checks will be faded to 3 random checks per week. Step 3) Phone checks will be faded to one random check per week. Step 4) Checks will be faded to one random check per month. Step 5) Full access restored
Support/Objective: (S4) John will be supported to purchase adult print media; (S5) John will be educated on safe and hygienic masturbation practices; (S6) John will be provided with easy read material on sexuality.
Useful Documents
Transition Template
Restoration Plan
Consultative Readiness Scale
988 Suicide Crisis Lifeline