Our goal of building a value-based purchasing (VBP) model is to improve quality and health for our members and lower cost.
Traditional Fee-for-Service
| 
| Value-Based Purchasing
|
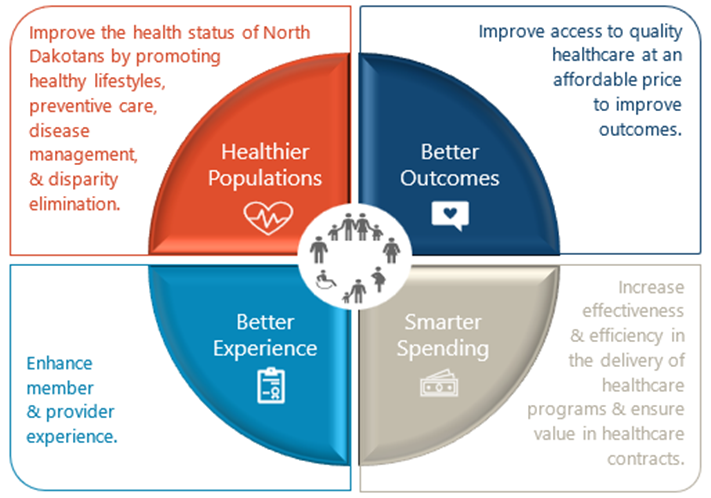
Program Strategy
Our program strategy consists of four components:
Program Overview
Program Start Date: July 1st, 2023
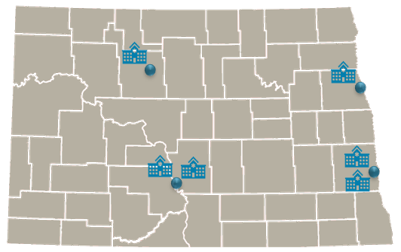
6 Prospective Payment System (PPS) Health Systems are mandatory participants in the model: Sanford Bismarck, Sanford Fargo, Altru Health System, CHI St. Alexius, Essentia Health and Trinity Health.
The PPS Hospital System VBP Program puts a portion of hospital payments at risk for performance on a suite of quality measures for their ND Medicaid patient population.
PPS Hospital Systems will see no loss of funding if they meet specific success criteria.
Quality Performance
Within the VBP Program, there are five priority health care domains included to improve population health. All measures selected align to these domain areas.
- Primary Care Access and Preventive Care
- Maternal Health Services
- Behavioral Health Services
- Care of Acute and Chronic Conditions
- Oral Health Services
The Quality Performance for each program year is outlined below:
What is pay for performance?
Starting in 2025, Health system performance will be evaluated against the Statewide Target as well as their own historical performance. The Statewide Target is defined as the highest level of performance that the Department wishes to achieve across the state in order to provide high quality care to all North Dakotans. Statewide Targets will be selected for each measure except structural measures which will be rated as met/not met.
Statewide targets will be set based on availability and a reasonable, incremental rate of change according to the following hierarchy based:
- Utilize the National HEDIS 50th percentile, or other applicable increment.
- Utilize the National Adult or Child Core Median.
- Utilize Regional data, as available.
- Utilize State-selected Target or Improvement over self.
Contact Information
Medical Services Division
North Dakota Health and Human Services
600 E. Boulevard Ave., Dept. 325
Bismarck, ND 58505-0250
Email: dhsmedicaidquality@nd.gov
